Mother-to-child transmission of HIV remains the most significant source of infection among children under 15 years of age. However, nearly all of these transmissions are preventable. In Kinshasa, the capital of the Democratic Republic of Congo, Doctors Without Borders (MSF) teams have established a dedicated healthcare program to prevent these infections.
In the DRC, it is estimated that around 452,914 people are living with HIV. While the virus is primarily transmitted through sexual contact, it can also be transmitted from mother to child during pregnancy, childbirth, or breastfeeding if the mother is HIV positive.
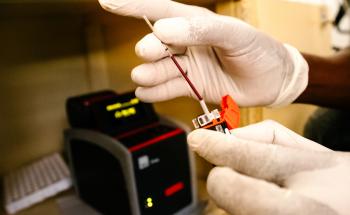
“Prevention of mother-to-child transmission (PMTCT) is a crucial part of the fight against HIV,” explains Gisèle Mucinya, medical manager of the HIV project in Kinshasa. “It involves testing pregnant women for HIV early in their pregnancy, providing immediate treatment if they test positive, and monitoring them throughout pregnancy, childbirth, and breastfeeding. Additionally, children born to HIV-positive mothers should be screened for HIV at six weeks after birth, receive preventive treatment, and be monitored until the final HIV test at 18 months. Although these steps are not extremely complex or expensive, their implementation remains challenging in the DRC.”

Although activities to prevent mother-to-child transmission of HIV (PMTCT) are officially integrated into the Congolese health system, the results regarding the protection of newborns remain very insufficient. Only 38 per cent of pregnant women who accessed prenatal consultations were tested for HIV. Among those tested and found to be HIV positive, only 58 per cent received antiretroviral (ARV) treatment. Additionally, nearly 60 per cent of babies exposed to HIV did not benefit from early detection tests.
The “One-stop shop”: An effective prevention model
One reason for these poor results is the fragmentation of PMTCT services that HIV-positive women must navigate to prevent transmission. Many mothers find themselves having to visit multiple service points for screening, treatment during pregnancy, treatment during breastfeeding, and treatment for their child. Gisèle Mucinya notes, “It’s an obstacle course, and many end up not accessing all the necessary services to prevent transmission.”
In response to this issue, MSF has been developing a care model recommended by the World Health Organization (WHO) aimed at ending service fragmentation since 2020. Known as the “One-Stop Shop PMTCT,” this integrated model is implemented in six healthcare facilities in Kinshasa. Here, pregnant or breastfeeding women who test positive for HIV, along with their exposed babies, receive all necessary care in one location.

“Everything is centralised: HIV detection, medication intake, monitoring throughout pregnancy and breastfeeding, screening the baby from birth, and overseeing the baby's care up to 18 months after birth,” explains Dorothée Tokula, a midwife at the Biyela Hospital Centre. “All of this is managed by the same medical staff, which enhances confidentiality and reduces care abandonment.”
Elodie, a twenty-year-old expectant mother, is a few months into her pregnancy under the care of the maternity ward at Biyela Hospital, supported by MSF. For her, the “One-stop shop for Prevention of Mother-to-Child Transmission (PMTCT)” instils hope for an HIV-free birth.
“I am in my second pregnancy. My first son was born here. I followed all the treatment processes during my pregnancy and after his birth, and he is currently HIV negative. I am grateful for the opportunity to give birth to uninfected children. At the moment, I am adhering to my treatment to ensure the health of the baby I am currently carrying. I want to encourage other HIV-positive mothers to know that it's possible for their babies to be born HIV-free if they follow their treatment correctly,” she says.
My first son was born here. I followed all the treatment processes during my pregnancy and after his birth, and he is currently HIV negative. I am grateful for the opportunity to give birth to uninfected children.Elodie, a twenty-year-old expectant mother in DRC
The results from this model are significant: 95 per cent of women enrolled in the One-stop shop PMTCT have given birth to children who did not contract HIV. The remaining 5 per cent arrived at the facilities late, and their babies had already contracted the virus. Additionally, all women followed through this model maintain an undetectable viral load due to their adherence to care.
“It’s a model that truly proves itself,” adds Dorothée. “I was familiar with the decentralised PMTCT model where care services were not provided in one location, leading to a high rate of care abandonment among HIV-positive pregnant women. It was very cumbersome, and confidentiality was not guaranteed. Now, everything has changed. Women feel secure and supported; they adhere easily to their treatment, resulting in children being born without HIV.”
It is indeed possible to give birth to a child without HIV, even if you carry the virus. As the world aims for an AIDS-free generation by 2030, the “One-stop shop PTME” model is demonstrating effectiveness in significantly reducing or even eradicating the transmission of HIV from mother to child. Today, MSF advocates for its inclusion in the financing plan and the national strategy to combat HIV in the DRC.