People bitten by snakes typically live in tropical or subtropical countries where venomous species are endemic. Those most at risk include farmers or rural communities that depend on agriculture or subsistence hunting and gathering. With its highly agrarian economy, India is the region most affected by snake bites, followed by sub-Saharan Africa.
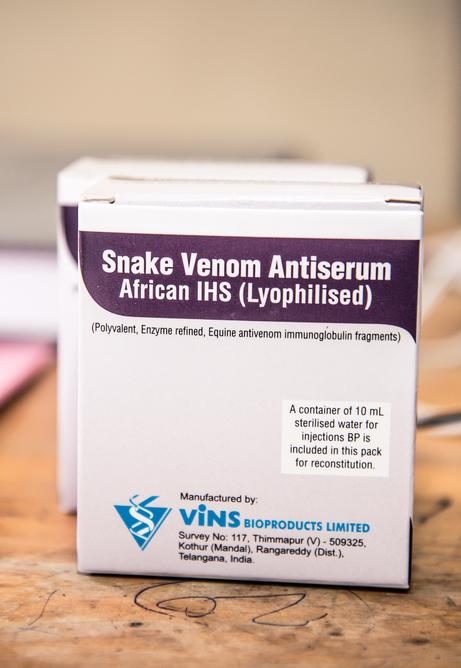
The risk of death or permanent disabilities is increased in remote communities where access to care is poor, as it is in many regions with highly venomous snakes. This limited access may reflect the lack of effective, affordable antivenoms available, of health workers trained in treating snake bites, or of nearby health facilities, or ambulances that can transport patients to health facilities, so they can receive care quickly after being bitten.
For these reasons, many victims turn to traditional healers, or to ineffective traditional medicines or low-quality antidotes. Young children under five have a higher risk of death, due to their lower body mass.